Abstract
Background: Although most patients with newly diagnosed acute myeloid leukemia (AML) obtain a complete remission (CR) following induction chemotherapy, most subsequently relapse. Previous studies have demonstrated the importance of various prognostic factors for relapse-free survival, including age, cytogenetics, prior antecedent hematologic disorder (AHD), and prior cancer-related therapy. However, assessments of treatment response now include additional factors such as measurable residual disease (MRD) status, time to count recovery, and remission type (CR vs. CR with incomplete count recovery [CRi]). Among patients in complete remission, we set out to examine the impact of additional initial response variables on relapse or death at various time points up to 3 years, a time point after which AML relapses become very uncommon.
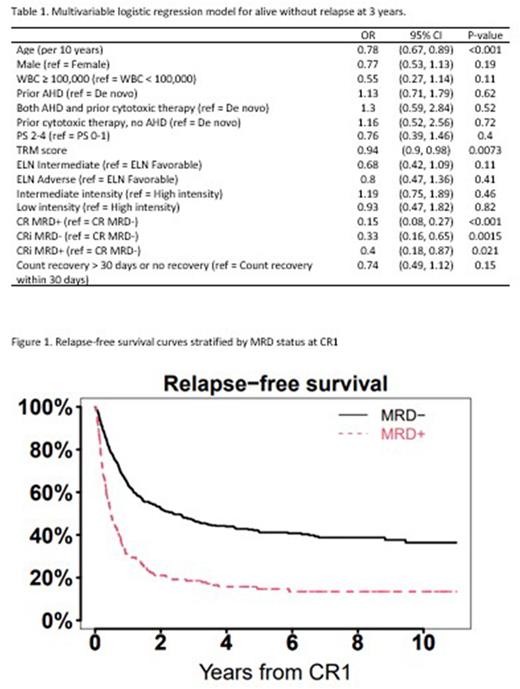
Methods: Of 972 patients who had a confirmed diagnosis of AML or other high-grade myeloid neoplasm (≥10% blasts) underwent initial induction treatment at University of Washington / Fred Hutchinson Cancer Center between November 2008 and December 2018, 656 achieved a morphologic remission (CR or CRi) and were included in our analysis. The primary outcomes were survival without relapse after 1, 2, or 3 years. Multivariable logistic regression models controlled for the following covariates: age, ELN 2017 risk classification, presence of MRD determined by multiparameter flow cytometry at first remission, gender, WBC count at diagnosis, prior AHD and/or therapy-related disease, performance status, treatment-related mortality (TRM) score, induction intensity (high: CLAG-M, FLAG-ida, or similar; intermediate: 7+3 or similar; low: hypomethylating agent with or without venetoclax), CR vs CRi, and count recovery within 30 days. Time to relapse was estimated using relapse-free survival curves.
Results: The median age at diagnosis was 60 years (range 18-91). De novo AML was found in 373 patients (57%) with the remainder a mix of antecedent AHD and therapy-related AML. ELN2017 risk classification was favorable in 181 patients (28%), intermediate in 206 (41%), and adverse in 203 (31%). Performance status was 0-1 in 538 patients (82%). Most patients received high or intermediate-intensity induction (88%). After induction, 540 patients (82%) achieved a CR and 116 patients (18%) CRi. MRD following induction therapy was found in 173 patients (26%). In multivariable analysis, age, remission type (CRi), and MRD status were the strongest predictors of being alive without relapse at years 1, 2, and 3 (year 3 summarized in Table 1). In the year 3 model, CR MRD+ after induction was associated with the largest decrease in odds of being alive without relapse (CR MRD+: odds ratio [OR] 0.15, 95% confidence interval [CI] 0.08-0.27). 3-year relapse-free survival (RFS) of 18.5% (95% CI 13.5-25.5%) for MRD+ patients versus 36.4% (95% CI 31.3-42.4%) for MRD- patients (Figure 1). CRi MRD+/MRD- were both also associated with decreased survival with CRi MRD- (OR 0.33, 95% CI 0.16-0.65) and CRi MRD+ (OR 0.40, 95% CI 0.18-0.87). Increasing age was the second strongest predictor across the models (year 3 OR 0.78, 95% CI 0.67-0.89).
Conclusions: Our study identified remission category (CR vs CRi), MRD status, and age as the strongest predictors of being alive without relapse at years 1, 2, or year 3 following induction for patients with AML and other high-grade myeloid neoplasms. Patients with older age or those with evidence of residual detectable disease with MRD or CRi and/or MRD have an increased risk of relapse or death in the first 3 years after initial CR.
Disclosures
Othus:Merck: Consultancy; Celgene: Consultancy; Biosight: Consultancy; Glycomimetics: Consultancy; Daiichi Sankyo: Consultancy. Halpern:Karyopharm Therapeutics: Research Funding; Incyte Pharmaceuticals: Research Funding; Jazz Pharmaceuticals: Research Funding; Gilead Sciences: Research Funding; Imago Biosciences: Research Funding; Novartis: Research Funding; Tolero Pharmaceuticals: Research Funding; Bayer Pharmaceuticals: Research Funding; Abbvie: Consultancy; Notable Labs: Consultancy. Walter:MacroGenics: Consultancy, Research Funding; Amphivena Therapeutics, Inc: Current equity holder in publicly-traded company; Aptevo Therapeutics: Consultancy, Research Funding; Pfizer, Inc: Consultancy, Research Funding; Selvita: Research Funding; Kite Pharma, Inc: Consultancy; Amgen: Consultancy, Research Funding; Kura Oncology: Consultancy, Research Funding; Kronos Bio, Inc: Consultancy; New Link Genetics: Consultancy; Jazz Pharmaceuticals: Consultancy, Research Funding; Janssen Research and Development: Research Funding; Janssen Global Services, LLC: Consultancy; ImmunoGen: Research Funding; GSK: Consultancy; Genentech: Consultancy; Celgene, Inc: Consultancy, Research Funding; Bristol Myers Squibb, Inc: Consultancy; Boston Biomedical, Inc: Consultancy; BioLineRx, LTd: Consultancy, Research Funding; Astellas Pharma US, Inc: Consultancy; Arog Pharmaceuticals: Research Funding; Agios: Consultancy, Research Funding; Race Oncology LTD: Consultancy; Stemline Therapeutics: Research Funding; AbbVie: Consultancy; BerGenBio, ASA: Consultancy; Orum Therapeutics, Inc.: Consultancy. Percival:Trillium: Research Funding; Abbvie: Research Funding; Celgene/BMS: Research Funding; Biosight: Research Funding; Glycomimetics: Research Funding; Cardiff Oncology: Research Funding; Oscotec: Research Funding; Pfizer: Research Funding; Ascentage: Research Funding; Telios: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal